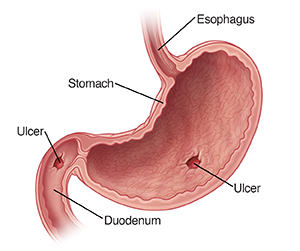
A peptic ulcer is an open sore in the lining of the stomach. It may also occur in the lower esophagus or first part of the small intestine (duodenum or jejunum). It's caused by a break in the protective lining of your stomach.
Causes
The most common causes of ulcers are:
-
H. pylori bacterial infection.
-
Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs). These include aspirin and ibuprofen.
-
Certain medicines like corticosteroids, bisphosphonates, potassium chloride, and fluorouracil.
-
Rare causes include:
-
Stress, as from acute illness, burns, or a head injury.
-
Viral infection.
-
Radiation therapy.
-
Crohn's disease.
-
Chemotherapy.
-
Cancers (gastric/lung cancer, lymphomas).
-
Factors that can increase the risk for ulcers include older age and a family history of peptic ulcers. Tobacco and alcohol use are also risk factors. Emotional stress, worry, and spicy foods don't cause peptic ulcers.
Symptoms
A peptic ulcer may or may not cause symptoms. If symptoms do occur, they can include:
-
Dull or burning pain anywhere between your belly button and breastbone. This can happen within 15 to 30 minutes after a meal. The pain can get worse 2 to 3 hours after a meal.
-
Loss of appetite.
-
Heartburn or upset stomach.
-
Frequent burping.
-
Bloated feeling.
-
Nausea or vomiting. Vomit may be bloody or look like coffee grounds.
-
Black, tarry, or bloody stools. This means the ulcer is bleeding.
-
Weight loss.
Sometimes the bleeding is not seen. In these cases, it may be discovered by symptoms of low blood count (anemia). These include dizziness, weakness, shortness of breath, pale skin, or trouble with exercise.
Without treatment, a peptic ulcer may get worse. This can lead to serious problems, such as bleeding, blockage, or a hole (perforation) in the stomach or duodenum.
Diagnosis
Tests to check for peptic ulcers include:
-
An upper endoscopy (EGD) is usually done to view the stomach lining and take samples (biopsies) to be examined under a microscope.
-
An X-ray test called an upper gastrointestinal (GI) series can be done in some cases. But it could miss small ulcers that would be seen on the upper endoscopy. It is done in people who cannot have EGD.
-
Blood tests.
-
Testing for H. pylori bacteria includes:
-
Urea breath test.
-
Stool antigen test.
-
Antibodies in blood.
-
Urine test.
-
-
Computerized tomography (CT) of the abdomen (belly) with contrast. This helps diagnose problems like perforation.
Home care
Medicines
Medicines are the most common treatment for peptic ulcers. In severe cases, surgery may be needed.
If you’re prescribed medicines, be sure to take them as directed. Common medicines include:
-
Antibiotics. These kill H. pylori bacteria. In many cases, you’ll need to take at least 2 types of antibiotics. The treatment schedules can be complicated and involve taking medicines either all at once or taken in order. This is because H. pylori infection is often hard to treat. It's very important to take the medicines as prescribed.
-
Proton pump inhibitors (PPIs). These block your stomach from making any acid. They provide relief from symptoms and help with healing. Calcium supplements may be added if you will be on PPI therapy for a long time. They reduce the risk of bone fractures.
-
H2 blockers. These reduce the amount of acid your stomach makes. They are sometimes used for duodenal ulcers.
-
Bismuth subsalicylate. This helps protect the lining of your stomach and duodenum from acid.
-
Carafate. This coats the stomach lining to protect it and help with healing.
General care
-
Don’t take aspirin or any NSAIDS, such as ibuprofen or naproxen, without talking with your health care provider first. They may delay healing. Also check with your provider before taking any antacids.
-
Don't consume caffeinated drinks, alcohol, or tobacco. These may delay healing and make symptoms worse.
-
Try to get to a healthy weight is strongly linked to peptic ulcer disease. Consult a registered dietitian nutritionist for help planning a healthy diet.
-
Work with your provider to find ways to reduce stress.
Follow-up care
Follow up with your healthcare provider as directed. If testing was done, you’ll be told the results when they are ready. In some cases of gastric ulcer, a repeat upper endoscopy is needed to check for healing. You may also need a test after treatment for H. pylori to confirm that you are infection-free.
When to get medical care
Call your health care provider right away if:
-
You have a fever of 100.4°F (38°C) or higher, or as advised by your provider.
-
You have stomach pain that gets worse.
-
You continue to lose weight.
-
You have pale skin.
-
You have extreme tiredness (fatigue).
-
You have trouble swallowing.
-
You have frequent vomiting, blood in your vomit, or a substance that looks like coffee grounds in your vomit.
-
You have black, tarry, or bloody stools.
-
You lose weight without trying.
Call 911
Call
-
You have sudden or severe pain in the stomach area.
-
Your stomach becomes rigid.
-
You have low body temperature.
-
Your heart rate is unusually fast.
-
Chest pain appears or gets worse, or spreads to the back, neck, shoulder, or arm.
-
You have shortness of breath or trouble breathing.
-
You have confusion.
-
You're extremely drowsy or have trouble waking up.
-
You faint.
-
You feel weak or dizzy.
-
There's a large amount of blood in your vomit or stool.