Your healthcare provider advises that you have a cerclage. This procedure closes the cervix during a pregnancy. It's done to help prevent miscarriage or premature birth. Abdominal cerclage involves making 1 or more cuts (incisions) in the belly (abdomen) to reach the cervix. The cervix is then stitched closed.
The cervix and pregnancy
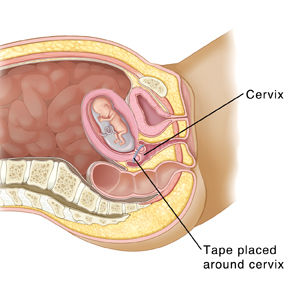
The uterus (womb) is where the baby grows during pregnancy. The cervix is the opening from the uterus to the vagina. The cervix normally remains firmly closed until the baby is ready to be born. A short or weakened cervix may not be able to stay closed as the baby grows larger. This is called cervical insufficiency or cervical incompetence. If the cervix fails and opens too soon, miscarriage or premature birth may result.
How abdominal cerclage works
The goal of cerclage is to hold the cervix closed. This allows the baby to fully develop before leaving the womb. Abdominal cerclage is done when other procedures to close the cervix have failed. It is done at about week 12 of pregnancy. The healthcare provider reaches the cervix through the abdomen. The cervix is then stitched closed. Following the procedure, you must give birth by cesarean section. Future births will also need to be by cesarean section.
Risks and possible complications of abdominal cerclage
The procedure is considered safe. But like all procedures, it carries some risks. These include the following:
-
Bleeding
-
Infection
-
Premature contractions
-
Premature labor or delivery
-
Premature rupture of membranes
-
Pregnancy loss
-
Cervix tears or ruptures
-
Injury to bladder or other nearby organs
-
Risks of anesthesia
Getting ready for the procedure
Tips for getting ready include:
-
Tell your healthcare provider about all medicines you take. This includes over-the-counter medicines like vitamins and pain medicines.
-
Don't put anything in your vagina for 24 hours before the procedure. This includes having sex.
-
Follow any directions you are given for not eating or drinking (including water) after midnight the night before the procedure. (If you have diabetes, ask your provider if you need special preparations.)
The day of the procedure
Here is what to expect on the day of the procedure:
-
Just before the procedure starts, an IV (intravenous) line is placed in your hand or arm. It delivers fluids and medicine into the body.
-
You will be given medicine (anesthesia) to keep you free of pain during the procedure. Depending on what type of anesthesia you get, you may be relaxed, drowsy, or fully asleep during the procedure.
-
The surgery may be done using either open surgery or laparoscopy.
-
Open surgery. One larger incision is made in the abdomen. The healthcare provider sees and works through this incision.
-
Laparoscopy. The provider makes 2 to 4 small incisions in the abdomen. A thin lighted tube called a laparoscope is then used. The scope allows the provider to work through the small incisions. The scope is put through 1 of the incisions. The scope sends pictures of the abdomen to a video screen. This lets the provider see inside the abdomen. Surgical tools are placed through the other small incisions. The abdomen is filled with carbon dioxide. This gas makes space for the healthcare provider to see and work.
-
-
For either method:
-
Surgical tools are used to release (cut) the tissue that connects the bladder and the lower part of the uterus, including the cervix. This gives access to the cervix.
-
A special surgical tape is wrapped around the cervix. The tape is tied in a knot.
-
The incision is closed with stitches or staples. A tube may be placed in the incision to drain fluids. It will be removed after that.
-
After the procedure
Here is what to expect after the procedure:
-
You will be taken to a room where you’ll recover from the anesthesia. Nurses will check on you as you rest.
-
You will be watched for signs of premature labor. You will also be given medicine that helps prevent premature labor.
-
Your baby’s heart rate will be watched.
-
You will have some light bleeding and cramping. This is normal. You will likely be given pain medicine. If you are still in pain, tell the nurse.
-
You may be able to go home later that day. Or you may stay overnight in a hospital room to be sure you don't go into premature labor. When you leave the hospital, have an adult friend or family member drive you home.
Recovering at home
Here is what to expect during home recovery:
-
You will likely be prescribed pain medicine to take at home. You may also be prescribed medicine to prevent labor. Take any medicine as prescribed.
-
Take it easy for 4 to 5 days after the procedure. Plan to have others help you as needed. If instructed to do so, you will need to stay in bed. Otherwise, you can get out of bed and do light activities.
-
Don't have sex until your healthcare provider says you can. This will likely not be until 2 to 6 weeks after the procedure.
-
Ask your provider when you can return to work and exercise.
-
Care for your incision as instructed by your provider You will have a dressing (bandage). Be sure you have instructions for when and how to change the dressing. Also be sure you know if you can get the incision wet when you bathe. If you have a drain that was not removed in the hospital, be sure you know how to care for it at home.
When to call the healthcare provider
Call your healthcare provider if you notice any of the following:
-
A fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Pain that doesn't go away even after taking pain medicine
-
Contractions that get worse or belly cramping
-
Unexpected vaginal spotting or bleeding
-
Fluid leaking from the vagina
-
Bad-smelling fluid leaking from the vagina
-
Back or belly pain
-
Signs of infection at the incision site or sites, such as redness or swelling, warmth, worsening pain, or bad-smelling drainage
Follow-up
Make a follow-up appointment, or as directed. During your follow-up visit, your healthcare provider will check your healing. You can also talk about how your pregnancy is going.