An ultrasound is a type of imaging test. It uses high-frequency sound waves, not radiation, to make images of the inside of your body. The images are seen on a computer screen.
Ultrasound can be used to look at the prostate gland. The prostate is part of the male reproductive system. This gland sits just under the bladder and in front of the rectum.
When ultrasound is used
You may need a prostate ultrasound (also called a transrectal ultrasound or TRUS) if your healthcare provider thinks you may have a problem with your prostate.
This is often used to look for prostate cancer. It is often done if your provider felt a lump or hard spot on your prostate during a digital rectal exam (DRE). Or it might be done if blood tests show you have a high or rising prostate-specific antigen (PSA) level. DRE and PSA tests are screening tests used to check for prostate cancer in men who have no symptoms of it.
Prostate ultrasound might be used to help find out why a man is having fertility problems.
It can also be used to see if the prostate is bigger than it should be. This is called BPH (benign prostatic hyperplasia). It's common in older men. BPH can cause problems passing and controlling urine. But it is not cancerous.
How ultrasound helps
Ultrasound uses sound waves to make images of the prostate gland. It helps your healthcare provider see if the gland looks normal.
It can also be used to help guide a biopsy. For a biopsy, tiny pieces of tissue are taken out and tested for cancer. A prostate biopsy is done with a needle. Ultrasound helps your provider guide the needle into the prostate and take out some of the changed part of the prostate that might be cancer.
If you have prostate cancer, you may choose to treat it with radiation therapy. It might be external or internal radiation. Internal radiation is also called brachytherapy. Ultrasound can be used to help your provider see exactly where to direct the placement of radioactive pellets in the prostate. .
Before the test
You may be told to use an enema or suppository the night or morning before a prostate ultrasound. This is to clean the stool out of your rectum to better view the prostate.
If a biopsy may be done, you might be asked to stop taking blood-thinning medicines, like warfarin or aspirin, for 1 week or so before the test. This helps lower the risk of bleeding. You might also be given antibiotics before and after the test. This helps prevent infection.
Carefully follow all of the instructions your provider gives you before the ultrasound.
During the test
What happens during the ultrasound:
-
Ultrasound is done by a specially trained technologist called a sonographer. The ultrasound may be done in your healthcare provider's office. It takes about 15 to 30 minutes.
-
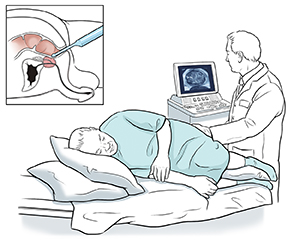
You'll be asked to change into a hospital gown. You'll then lie on your side with your knees bent up toward your chest.
-
The test is done with a hand-held ultrasound probe. A disposable cover is put on the probe. The probe is a tube-shaped rod about the size of a finger. A gel is put on the probe to grease (lubricate) it.
-
Your healthcare provider gently puts the probe into your rectum. You'll feel pressure, but if it hurts, let your provider know.
-
Sound waves are sent into the probe and through the wall of your rectum. They bounce off your prostate. A computer uses them to form an image of the gland and nearby tissues.
-
Your provider looks at the image and checks the size and shape of your prostate.
-
If changes are seen in any part of your prostate, a biopsy might be done. This is often done by a urologist. To do this, a thin, hollow needle is put through your rectum and into your prostate gland. Small bits of the changed area fill the needle (a core) and are taken out for testing. You may feel pressure when this is done and only brief discomfort. But it usually doesn't hurt. You might want to ask your provider if there are plans to numb the area near the prostate with a local anesthetic. Several samples (often 12 or more) are collected from different parts of the prostate.
-
When the test is done, the probe is removed.
-
You can go home the same day, and go back to your normal activities.
-
If a biopsy was done, you may be given a thin pad to wear in case of bleeding. You may see blood in your urine, semen, or stool for a day or so. This is normal. You may have some discomfort for a few days. It might be worse when sitting.
After the test
Talk with your provider about how and when you'll get your test results and what happens next.