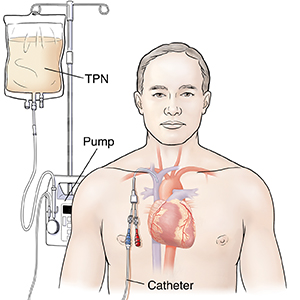
You are going home on total parenteral nutrition (TPN). TPN is a way for you to get nutrition through a tube (catheter) in your vein. The TPN solution has the vitamins, minerals, and other nutrition you normally get by eating food. Your health care provider will decide if you can also eat food while you are on TPN.
In the hospital, you learned how to take care of your catheter and how to infuse your TPN. At home, you will need to do these tasks:
-
Use the infusion pump that sends the TPN into your veins.
-
Start and stop your TPN infusion.
-
Flush the catheter.
-
Prevent problems or fix any problems that occur.
-
Care for your catheter.
-
Care for your pump.
You will work closely with a nurse until you feel comfortable taking care of your catheter and giving yourself TPN.
The information below gives you a general overview of TPN. It has reminders and tips about what you’ll need to do each day. Ask your provider for more information about caring for your catheter, using sterile technique, adding medicines to your solution, and flushing your catheter. Other instruction sheets are available to guide you.
Preparing your work area
-
Choose a work area away from household traffic. Keep pets and children out of the room. Don’t work in the bathroom. It has too many germs.
-
Collect your supplies. You were shown at the hospital which supplies you need. The nurse will show you how to organize what you need each day.
-
Clean your work area like this:
-
Clean washable surfaces with soap and water. Dry the surface with a clean paper towel.
-
Wipe dust off surfaces that are not washable, such as wood. Spread a clean cloth or paper towels over the surface.
-
If you need to cough or sneeze, move away from the clean surface.
-
Washing your hands
Wash your hands before touching any of your supplies. To do this:
-
Turn on the water.
-
Wet your hands and wrists.
-
Squirt antibacterial soap from a pump dispenser into your hands and work up a good lather.
-
Scrub your hands thoroughly. Do this for at least 2 minutes.
-
Rinse your hands with your fingers pointing downward. Allow the water to run down from your wrists to your fingertips. This way, the dirty water flows downward.
-
Dry your hands with a paper towel. Turn off the faucet with this towel.
-
When you have washed your hands, don’t touch anything except your catheter and supplies. You must wash your hands again if you touch anything else, such as furniture or your clothes.
Caring for your solution
-
Keep your solution refrigerated when not in use.
-
Check the label on the bag to make sure it matches your prescription exactly. Don’t use the bag if it does not match the prescription. Contact your supply company or your TPN nurse.
-
Check the expiration date. Don’t use the solution if it is past the expiration date. Get a new bag from the refrigerator.
-
Check the bag for problems. These include leaks, cloudiness, or things floating in it. Don’t use the bag if you see any of these things. Get a new bag from the refrigerator.
-
Warm the TPN solution by leaving it at room temperature for 1 hour before use. Never put the bag in the microwave.
-
Add any additional medicines or vitamins to the bag before you infuse the solution. Follow the nurse's directions for starting and ending the TPN, including how to discard used supplies.
Follow-up care
-
You will work closely with a home health nurse or TPN nurse.
-
Follow up with your health care provider, or as advised.
When to contact your doctor
Contact your health care provider or get medical care right away if you have any of these:
-
Excessive thirst
-
Upset stomach (nausea) or vomiting
-
Weakness or shakiness
-
Fainting or feeling like you may faint
-
Sweating
-
Headache
-
Belly (abdominal) pain
-
Sudden weight loss or gain (more than 2 pounds in 24 hours)
-
Fever above 100.4°F (38°C) or higher, or as directed by your provider
-
Shaking chills
-
Redness, swelling, or warmth at your insertion site
-
Fluid or pus coming from your insertion site
Call 911
Call
-
Shortness of breath
-
Heart palpitations
-
Chest pain