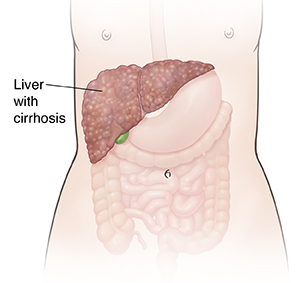
The liver is found on the right side of your belly (abdomen). It's just below the rib cage. The liver has many important jobs. It removes toxins from the blood. It also makes important proteins that help your blood clot when you are wounded. Cirrhosis is scarring of the liver. It happens over time from chronic liver injury. This damage is permanent. It can cause your liver to stop working (liver failure).
The most common causes of cirrhosis are long-term heavy alcohol use and chronic hepatitis B or C. There are many other causes. The most common one used to be called nonalcoholic fatty liver disease and is now called metabolic dysfunction-associated steatotic liver disease. Other causes include autoimmune diseases targeting the liver, inherited liver diseases, such as Wilson disease and hemochromatosis, a variety of toxins or long-term use of certain medicines. Diseases that damage, destroy, or block bile ducts in the liver can also cause cirrhosis.
Common symptoms of cirrhosis include:
-
Tiredness or weakness
-
Loss of appetite
-
Nausea and vomiting
-
Easy bleeding and bruising
-
Swelling of the belly (abdomen), lower legs, ankles, or feet
-
Weight loss
-
Yellowing of the eyes or skin (jaundice), pale or clay-colored stools, and dark yellow urine
-
Itching
-
Redness on the palms of the hands
-
Confusion
Treatment helps ease symptoms and prevent more liver damage. You may also get treatment to cure hepatitis C and treat hepatitis B. Quitting alcohol will help stop the disease from getting worse. It may also prevent complications. If cirrhosis gets worse and becomes life-threatening, you may need a liver transplant.
Home care
-
Don't take medicines that can make liver damage worse. Your healthcare provider will tell you if any of the medicines you take need to be changed. Talk with your provider or pharmacist before taking any medicine not prescribed. These include any over-the-counter medicines, dietary supplements, and herbs. Some of these may make liver damage worse.
-
Talk with your healthcare provider about medicines that have acetaminophen or NSAIDs, such as ibuprofen and naproxen. These can harm your liver and kidneys.
-
Stop drinking alcohol. If you find it hard to stop drinking, seek professional help. Consider joining Alcoholics Anonymous or another type of treatment program for support. Ask your providers for detoxification information or rehabilitation centers.
-
If you use IV drugs, you are at high risk for hepatitis B and C. Get help to stop.
-
Get regular exercise and maintain your weight in the normal range. Get help from your provider if this is difficult for you. Treat any underlying metabolic conditions. This is very important because metabolic conditions, such as obesity, high blood pressure, heart disease, diabetes, and high cholesterol can lead to liver disease or make it worse.
-
Be sure to ask your healthcare provider about recommended vaccines. Get vaccinated for pneumonia, influenza, hepatitis A and B, and shingles. These include vaccines for viruses that can cause liver disease.
Follow-up care
Follow up with your healthcare provider, or as advised. If you have cirrhosis, you may need testing to look for complications, including liver cancer. Keep follow-up appointments. Consistent tracking of your overall health and lab values is important.
For more information and to learn about support groups for people with liver disease, contact:
-
American Liver Foundation, www.liverfoundation.org
-
AASLD Foundation, www.aasldfoundation.org/patients
When to get medical advice
Call your healthcare provider right away if:
-
You rapidly gain weight, with increased size of your belly (abdomen) or leg swelling
-
Yellow color of your skin or eyes (jaundice) gets worse
-
You have excess bleeding from cuts or injuries
-
You have blood in your vomit or bleeding from your rectum