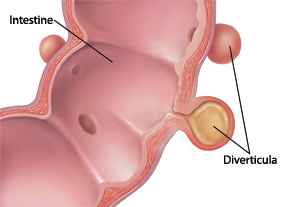
Some people as they get older get pouches that push into the wall of the colon. These pouches are called diverticuli. They often cause no symptoms. If the pouches become blocked, they can become inflamed and infected. This is called diverticulitis. It causes pain in your lower belly (abdomen) and fever. It may also cause nausea, vomiting, diarrhea, or constipation. If not treated, it can become a serious health problem. It can cause an abscess to form around the pouch. The abscess may block the intestinal tract. The pouch may even tear or rupture. This can spread infection throughout the belly. You will need emergency medical treatment if that happens.
Sometimes, diverticulitis may not need antibiotics. But antibiotics are most often used. When treatment is started early, oral antibiotics alone may be enough to cure diverticulitis. This method is tried first. But if you don't get better or if your condition gets worse while taking antibiotics, you may need to be admitted to the hospital. There, you will get antibiotics and fluids through an IV (intravenous) line. You may also have to rest your bowel. That means you won't eat or drink for a period of time. Severe cases may need surgery.
Home care
These guidelines will help you care for yourself at home:
-
During the acute illness, rest and follow your healthcare provider's instructions about diet. Sometimes you will need to be on a clear liquid diet to rest your bowel. Once your symptoms are better, you may be told to eat a low-fiber diet for some time. You can eat foods such as:
-
Flake cereal
-
Mashed potatoes
-
Pancakes and waffles
-
Pasta
-
White bread
-
Rice
-
Applesauce
-
Bananas
-
Eggs
-
Fish
-
Poultry
-
Tofu
-
Cooked soft vegetables
-
-
Take antibiotics exactly as told. Don't miss any doses or stop taking the medicine, even if you feel better.
-
Keep track of your temperature. Tell your healthcare provider if you have a rising temperature.
Preventing future attacks
Once you have an episode of diverticulitis, you are at risk of having it again. But you may be able to lower your risk by eating a high-fiber diet (20 g/day to 35 g/day of fiber). This cleans out the colon pouches that already exist. It may also prevent new ones from forming. Foods high in fiber include:
-
Fresh fruits and edible peelings
-
Raw or lightly cooked vegetables
-
Whole-grain cereals and breads
-
Dried beans and peas
-
Bran
Here are other steps you can take to help prevent future attacks:
-
Take your medicines, such as antibiotics, as your healthcare provider says.
-
Drink 6 to 8 glasses of water every day, unless told otherwise.
-
Use a heating pad or hot water bottle to help with belly cramping or pain.
-
Start an exercise program. Ask your healthcare provider how to get started. You can benefit from simple activities, such as walking or gardening.
-
Treat diarrhea with a bland diet. Start with liquids only. Then slowly add fiber over time.
-
Watch for changes in your bowel movements (constipation to diarrhea). Prevent constipation by eating a high-fiber diet, plenty of fluids, and taking a stool softener if needed.
-
Get plenty of rest and sleep.
-
Don't take NSAIDs (anti-inflammatory drugs) unless your healthcare provider tells you to. They can increase your risk for diverticulitis.
Follow-up care
Check in with your healthcare provider as advised or sooner if you are not getting better in the next 2 days. Your provider may advise a colonoscopy to look at the colon once it has healed.
When to call your healthcare provider
Call your healthcare provider right away if any of these occur:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Repeated vomiting or swelling of the belly
-
Weakness, dizziness, light-headedness
-
Pain in your belly that gets worse, is severe, or spreads to your back
-
Pain that moves to the right lower belly
-
Rectal bleeding. This means stools that are red, black, or maroon in color.
-
Unexpected vaginal bleeding or pus discharge
Featured in