The conjunctiva is a thin membrane that covers the eye and the inside of the eyelids. It can become irritated and inflamed. If no reason for this inflammation is found, it is called nonspecific conjunctivitis.
When the conjunctiva becomes inflamed, the eye looks red. Small blood vessels are visible up close. The eye may have a clear or white, cloudy discharge. The eyelids may be swollen and red. There may be morning crusting around the eye. Most likely, the conjunctivitis was caused by a brief irritation. The irritated eye is treated with a soothing nonprescription ointment or eye drops.
Home care
Medicines
The healthcare provider may prescribe medicine to ease eye irritation. Follow the healthcare provider’s instructions for giving this medicine to your child.
-
Wash your hands well with soap and warm water before and after caring for your child’s eye.
-
It is common for discharge to form crusts around the eye. Gently wipe crusts away with a wet swab or a clean, warm, damp washcloth. Wipe toward the ear. This is to keep the eye as clean as possible.
-
Try to prevent your child from rubbing the eye.
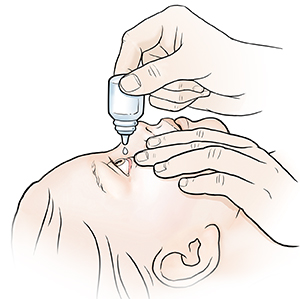
To apply ointment or eye drops:
-
Have your child lie down on their back.
-
Using eye drops. Apply drops in the corner of the eye, where the eyelid meets the nose. The drops will pool in this area. When your child blinks or opens their lids, the drops will flow into the eye. Give the exact number of drops prescribed. Be careful not to touch the eye or eyelashes with the dropper.
-
Using ointment. If both drops and ointment are prescribed, give the drops first. Wait 3 minutes, and then apply the ointment. Doing this will give each medicine time to work. To apply the ointment, start by gently pulling down the lower lid. Place a thin strip of ointment along the inside of the lid. Begin at the nose and move outward. Close the lid. Wipe away excess medicine from the nose outward. This is to keep the eye as clean as possible. Have your child keep the eye closed for 1 or 2 minutes so the medicine has time to coat the eye. Eye ointment may cause blurry vision. This is normal. Apply ointment right before your child goes to sleep. In infants, the ointment may be easier to apply while your child is sleeping.
-
Wipe away excess drops or ointment with a clean cloth.
Follow-up care
Follow up with your child’s healthcare provider as advised.
When to get medical advice
For a usually healthy child, call the healthcare provider right away if any of these occur:
-
Your child has a fever (see Fever and children section below).
-
Your child has increasing or continuing symptoms.
-
Your child has vision problems (not related to ointment use).
-
Your child shows signs of infection, such as increased redness or swelling, pain that gets worse, or foul-smelling drainage from the eye.
Call 911
Call
-
Your child has trouble breathing.
-
Your child shows confusion.
-
Your child is very drowsy or has trouble waking up.
-
Your child faints or loses consciousness.
-
Your child has a rapid heart rate.
-
Your child has a seizure.
-
Your child has a stiff neck.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
Featured in