Your child has an upper respiratory illness (also called an upper respiratory infection or URI). This means a common cold. It's caused by a virus and is contagious during the first few days. It's spread through the air by coughing or sneezing or by direct contact. This means by touching your sick child and then touching your own eyes, nose, or mouth. Washing your hands often will decrease risk of spreading the virus. Most viral illnesses go away within 7 to 14 days with rest and simple home care. But they may sometimes last up to 4 weeks.
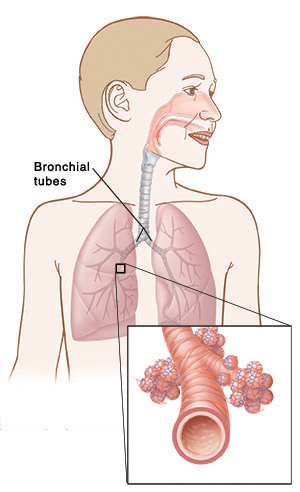
Antibiotics won't kill a virus and are generally not prescribed for conditions caused by a virus. If there is a lot of irritation, the air passages can go into spasm and cause wheezing even in children who don't have asthma. Medicine, such as a bronchodilator, may be prescribed to prevent wheezing.
Home care
-
Fluids. Fever increases water loss from the body. Encourage your child to drink lots of fluids to loosen lung secretions and make it easier to breathe.
-
For babies under 12 months, continue regular formula or breast feedings. Between feedings, give oral rehydration solution. You can buy this at drugstores and grocery stores without a prescription.
-
For children over 1 year old, give plenty of fluids, such as water, juice, gelatin water, soda without caffeine, ginger ale, lemonade, or ice pops.
-
-
Eating. If your child doesn't want to eat solid foods, it's okay for a few days, as long as they drink lots of fluid.
-
Rest. Keep children with a fever at home resting or playing quietly. Encourage frequent naps. Your child may return to daycare or school when the fever is gone and they are eating well and feeling better.
-
Sleep. Give your child plenty of time to sleep.
-
Children 1 year and older: Have your child sleep in a slightly upright position. This is to help make breathing easier. If you can, raise the head of the bed slightly. Or raise your older child’s head and upper body with extra pillows. Talk with your doctor about how far to raise your child's head.
-
Babies younger than 12 months: Never use pillows or put your baby to sleep on their stomach or side. Babies younger than 12 months should sleep on a flat surface on their back. Don't use car seats, strollers, swings, baby carriers, and baby slings for sleep. If your baby falls asleep in one of these, move them to a flat, firm surface as soon as you can.
-
-
Cough. Coughing is a normal part of this illness. A cool mist humidifier at the bedside may help. Clean the humidifier every day to prevent mold. Over-the-counter (OTC) cough and cold medicines have not proved to be any more helpful than syrup with no medicine in it. They also can produce serious side effects, especially in babies under 2 years of age. Don't give OTC cough or cold medicines to children under 6 years unless your doctor has specifically advised you to do so.
-
Keep your child away from cigarette smoke. Smoke can make the cough worse. Don't let anyone smoke in your house or car.
-
If your child takes any prescribed medicines, always talk with their doctor before giving them any OTC medicines, especially for the first time.
-
-
Nasal congestion. Suction the nose of babies with a bulb syringe. You may put 2 to 3 drops of saltwater (saline) nose drops in each nostril before suctioning. This helps thin and remove secretions. You can buy saline nose drops without a prescription. You can also use 1/4 teaspoon of table salt mixed well in 1 cup of water.
-
Fever. Use children’s acetaminophen for fever, fussiness, or discomfort, unless another medicine was prescribed. In babies over 6 months of age, you may use children’s ibuprofen or acetaminophen. If your child has chronic liver or kidney disease or has ever had a stomach ulcer or gastrointestinal bleeding, talk with the doctor before using these medicines. Don't give aspirin to children or teens unless your child’s doctor says it is safe. Aspirin can put your child at risk for Reye syndrome, a rare but serious condition.
-
Wheezing. If a bronchodilator medicine (inhaled spray, oral, or with a nebulizer) was prescribed, have your child take it exactly at the times advised. If your child needs this medicine more often (especially from a handheld inhaler or aerosol breathing medicine), this is a sign that the bronchospasm is getting worse. If this occurs, contact your doctor or return to this facility right away. It's also important to use the correct method when using a bronchodilator inhaler.
-
Preventing spread. Washing your hands before and after touching your sick child will help prevent a new infection. Good hand-washing will help keep the virus from spreading to you and to other children. Don't touch your eyes, nose, or mouth.
-
Education. In an age-appropriate manner, teach your children when, how, and why to wash their hands. Role model correct hand-washing. Encourage adults in your home to wash hands often. Help teach everyone in the home to not touch their eyes, nose, or mouth.
Follow-up care
Follow up with your child's doctor, or as advised.
When to get medical advice
Contact your child's doctor if your child has:
-
A fever (see Fever and children, below).
-
Any symptoms of dehydration, such as:
-
No tears when crying.
-
Sunken eyes or a dry mouth.
-
No wet diapers for 8 hours in infants.
-
Reduced urine output in older children.
-
-
An earache, sinus pain, a stiff or painful neck, a headache, repeated diarrhea, or vomiting.
-
Unusual fussiness.
-
A new rash.
-
New symptoms, or you are concerned about how your child is doing.
Call 911
Call
-
Has increased wheezing or trouble breathing.
-
Has unusual drowsiness or confusion.
-
Feels dizzy or faint.
-
Cannot talk or is unresponsive.
-
Has blue, purple, or gray lips or skin.
-
Has fast breathing. This means:
-
Birth to 6 weeks: over 60 breaths per minute.
-
6 weeks to 2 years: over 45 breaths per minute.
-
3 to 6 years: over 35 breaths per minute.
-
7 to 10 years: over 30 breaths per minute.
-
Older than 10 years: over 25 breaths per minute.
-
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The doctor may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The doctor may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it, and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel okay using a rectal thermometer, ask the doctor what type to use instead. When you talk with any doctor or nurse about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s doctor may give you different numbers for your child. Follow your doctor’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s doctor how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the doctor in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° F (38° C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
Featured in