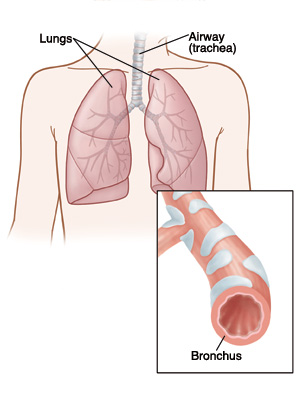
When your child breathes, the air goes down their main windpipe (trachea) and through the bronchi into the lungs. The bronchi are the 2 tubes that lead from the trachea to the left and right lungs. If the bronchi get irritated and inflamed, they can narrow. This is because the muscles around the air passages go into spasm. This makes it hard to breathe. This condition is called bronchospasm.
Bronchospasm can be caused by many things. These include allergies, asthma, a respiratory infection, exercise, or reaction to a medicine.
Bronchospasm makes it hard to breathe out. It causes wheezing when exhaling. In severe cases, it's hard to breathe in or out. Wheezing is a whistling sound caused by breathing through narrowed airways. Bronchospasm can also cause frequent coughing without the wheezing sound. A child with bronchospasm may cough, wheeze, or be short of breath. The inflamed area creates mucus. The mucus can partially block the airways. The chest muscles can tighten. The child can also have a fever.
A child with bronchospasm may be given medicine to take at home. A child with severe bronchospasm may need to stay in the hospital for one or more nights. There, they are given IV (intravenous) fluids, breathing treatments, and oxygen.
Children with asthma often get bronchospasm. But not all children with bronchospasm have asthma. If a child has repeated bouts of bronchospasm, then they may need to be tested for asthma.
Home care
Follow these guidelines when caring for your child at home:
-
Your child's healthcare provider may prescribe medicines. Follow all instructions for giving these to your child. Don’t give your child any medicines that have not been approved by the provider. Your child may be prescribed bronchodilator medicine. This is to help with breathing. It may come as an inhaler with a spacer, or a liquid that is made into an aerosol by a machine, then breathed in. Have your child use the medicine exactly at the times advised.
-
Don’t give a child under age 6 cough or cold medicine unless the healthcare provider tells you to do so.
-
Know the warning signs of a bronchospasm attack. These can include cough, wheezing, shortness of breath, chest tightness, irritability, restless sleep, fever, and cough. Your child may have no interest in feeding. Learn what medicines to give if you see these signs.
-
Wash your hands well with soap and clean, running water before and after caring for your child. This is to help prevent spreading infection.
-
Give your child plenty of time to rest.
-
Children 1 year and older: Have your child sleep in a slightly upright position. This is to help make breathing easier. If possible, raise the head of the bed slightly. Or raise your older child’s head and upper body up with extra pillows. Talk with your healthcare provider about how far to raise your child's head.
-
Babies younger than 12 months: Never use pillows or put your baby to sleep on their stomach or side. Babies younger than 12 months should sleep on a flat surface on their back. Don't use car seats, strollers, swings, baby carriers, and baby slings for sleep. If your baby falls asleep in one of these, move them to a flat, firm surface as soon as you can.
-
-
To prevent dehydration and help loosen lung mucus in toddlers and older children, have your child drink plenty of liquids. Children may prefer cold drinks, frozen desserts, or frozen ice pops. They may also like warm chicken soup or drinks with lemon and honey. Don’t give honey to a child younger than 1 year old.
-
To prevent dehydration and help loosen lung mucus in babies, have your child drink plenty of liquids. Use a medicine dropper, if needed, to give small amounts of breastmilk, formula, or clear liquids to your baby. Give 1 to 2 teaspoons every 10 to 15 minutes. A baby may only be able to feed for short amounts of time. If you are breastfeeding, pump and store milk to use later. Give your child oral rehydration solution between feedings. These are available from the drugstore.
-
Don’t smoke around your child. Tobacco smoke can make your child’s symptoms worse.
Follow-up care
Follow up with your child’s healthcare provider, or as advised.
Special note to parents
Don’t give cough and cold medicines to any child under age 6. These don't help young children, and they may cause serious side effects.
When to get medical care
Call your child's healthcare provider right away if any of these occur:
-
No improvement within 24 hours of treatment
-
Symptoms that don’t get better, or get worse
-
Cough with lots of thick colored mucus
-
Trouble breathing that doesn’t get better, or gets worse
-
Fast breathing
-
Loss of appetite or poor feeding
-
Signs of dehydration, such as dry mouth, crying with no tears, or peeing less than normal
-
More medicine than prescribed is needed to help relieve wheezing
-
The medicine doesn’t relieve wheezing
-
Fever (see "Fever and children" below)
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° F (38° C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
Author: Wheeler, Brooke
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.