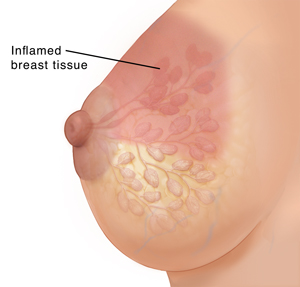
Mastitis occurs when breast tissue becomes swollen and inflamed. This is almost always due to infection. Mastitis most often affects breastfeeding women during the first 6 weeks after childbirth. For this reason, it’s also known as lactation mastitis. Infection may happen after a duct becomes clogged, causing milk to back up in the breast. Mastitis may also occur if bacteria enter the breast through small cracks in the nipple.
Less often, mastitis occurs in women who aren’t breastfeeding. If you have mastitis that is not due to breastfeeding, your healthcare provider will give you more information as needed. Treatment may include some of the same home care measures listed below.
Mastitis may cause flu-like symptoms such as fever, aches, and fatigue. The affected breast may feel painful, warm, tender, firm, or swollen. The skin over the breast may be red (often in a wedge-shaped pattern). You may feel a burning a sensation when breastfeeding.
In most cases, mastitis can be treated with antibiotics. This should clear the infection. If treatment is delayed, a pocket of pus (abscess) can form in the breast tissue. A procedure may then be needed to drain the pus. In severe cases of infection, other treatments may be needed.
Home care
Breastfeeding
-
It’s very important to keep the affected breast drained through routine breastfeeding or pumping sessions. Don't increase breast emptying beyond what the baby's feeding needs are. Overfeeding from the affected breast or ‘‘pumping to empty’’ continues a cycle of hyperlactation and is a major risk factor for tissue swelling and inflammation getting worse.
-
Tell your healthcare provider if you have problems with breastfeeding. They may suggest changes to your technique, if needed. You may also be referred to a lactation nurse or consultant for support with breastfeeding.
General care
-
Take any medicines you’re prescribed as directed. If you’re taking antibiotics, be sure to complete all of the medicine even if you start to feel better. Over-the-counter pain medicines may also be recommended. Don’t use breast creams or other products or medicines without talking to your healthcare provider first. If you’re concerned about taking medicines while breastfeeding, talk to your healthcare provider.
-
Rest as often as needed. Also be sure to drink plenty of fluids.
-
Gently massage the area. Stay away from deep massage, which can cause inflammation to get worse. Instead, consider light yet firm sweeping touch of the skin in the armpit or upper chestThis helps move fluid away from the ducts.
-
To help decrease inflammation, consider applying an ice pack wrapped in a thin towel every hour for 10 to 15 minutes at a time.
-
Wear a well-fitting bra that is not tight. Sometimes a tight bra constricts milk ducts and causes problems.
Follow-up care
Follow up with your healthcare provider as advised.
When to seek medical advice
Call your healthcare provider right away if any of these occur:
-
Fever of 100.4°F (38°C) or higher, or as directed by your provider
-
Shaking chills
-
Worsening symptoms or symptoms that don't improve within 48 to 72 hours of starting treatment
-
New symptoms develop