The tests you had show that you're pregnant. But the exact cause of your pain is not clear.
Some pain and bleeding are common in early pregnancy. Often they stop, and you can go on to have a normal pregnancy and baby. Other times the pain or bleeding can be signs of a miscarriage or ectopic pregnancy. An ectopic pregnancy is a very serious problem. It means that the fertilized egg attached (implanted) in a place other than inside the uterus. At this time, it's unclear if your pregnancy will continue normally, if you'll have a miscarriage, or if you could have an ectopic pregnancy. Below is some information about this.
Miscarriage
At this time, it's not known if you'll have a miscarriage, or if things will clear up and your pregnancy will continue normally. This is an emotionally difficult time. But it's important to understand that miscarriages are common.
About 1 or 2 out of 10 pregnancies end this way. Some end even before a person knows they're pregnant. This happens for many reasons. Often the cause is never found. But it’s important that you know it's not your fault. It didn’t happen because you did anything wrong.
Having sex or exercising doesn't cause a miscarriage. These activities are usually safe unless you have pain or bleeding or your doctor tells you to stop. Even minor falls won’t cause a miscarriage. Miscarriages happen because things weren't developing as they were supposed to. No medicine can prevent a miscarriage.
Ectopic pregnancy
In a normal pregnancy, the fertilized egg attaches to the wall of the uterus. In an ectopic pregnancy, the fertilized egg attaches outside the uterus, usually in the fallopian tube (tubal pregnancy). In very rare cases, the egg attaches to an ovary or somewhere else in the belly (abdomen). An ectopic pregnancy is much less common than a miscarriage. But it's very serious. The baby can't survive at a site other than the inside of the uterus. As the pregnancy progresses, the fallopian tube can burst (rupture). This can cause internal bleeding and even death. Risk factors for an ectopic pregnancy are:
-
A past ectopic pregnancy.
-
Pelvic inflammatory disease.
-
Endometriosis.
-
Smoking.
-
An IUD.
Additional tests
It's not known what's causing your symptoms. Your doctor will ask about your medical history and do a physical exam. You'll need more tests to figure out what the problem is. You may need the tests below.
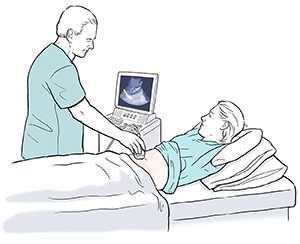
Ultrasound
An ultrasound can often find a normal pregnancy as early as 4 to 5 weeks. If the ultrasound does not show the baby inside the uterus, it means one of these things:
-
You have a normal pregnancy less than 4 weeks along.
-
You are having or recently had a miscarriage.
-
You have an ectopic pregnancy.
Pregnancy hormone
An HCG test measures the amount of HCG (a pregnancy hormone) in your blood. Comparing today's test result to a repeat test in 2 days will show if you have a normal pregnancy.
Laparoscopy
This is a type of surgery. The doctor will put a tube with a camera and light source inside your belly to look directly at your pelvic organs. This test is used when it's not safe to wait 2 days for blood test results.
Important information
If you do have an ectopic pregnancy, there's a small chance that the growing fetus can tear the fallopian tube. This can cause severe internal bleeding. If this happens, you may have:
-
Sudden severe pain in your lower belly.
-
Vaginal bleeding.
-
Weakness, dizziness, and sometimes fainting.
If any of these symptoms occur:
-
Call 911 or return right away to the hospital.
-
Don't drive yourself.
-
Don't go to your doctor's office or a clinic. Go to the hospital.
Home care
Follow these guidelines to help care for yourself at home:
-
Rest until your next exam. Don’t do any strenuous activities.
-
Eat a light diet with foods that are easy to digest.
-
Don’t have sex until your doctor says it’s okay.
-
Don't take any medicines without your doctor's approval.
Follow-up care
Follow up with your doctor, or as advised. If you were told to have a repeat blood test in 2 days, it’s important to get it done.
If you had an ultrasound, a radiologist will review it. You'll be told of any new findings that may affect your care.
Call 911
Call
-
Severe pain
-
Heavy bleeding
-
Severe lightheadedness, passing out, or fainting
-
Rapid heart rate
-
Trouble breathing
-
Confusion or trouble waking up
When to get medical care
Contact your doctor right away if:
-
The pain in your belly gets worse.
-
You're dizzy or weak when you stand.
-
You have heavy vaginal bleeding. This means soaking one pad an hour for 3 hours.
-
You have vaginal bleeding for more than 5 days.
-
You have repeated vomiting or diarrhea.
-
The pain in your belly moves to the lower right.
-
You have blood in your vomit or bowel movements. This will be dark red or black.
-
You have a fever of 100.4ºF (38ºC) or higher, or as advised by your doctor.