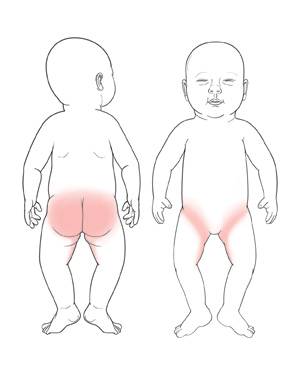
Candida is a type of yeast. It grows best in warm, moist areas. It's common for candida to grow in the skin folds under a child’s diaper. When there's an overgrowth of candida, it can cause a rash called a candida diaper rash.
The entire area under the diaper may be bright red. The borders of the rash may be raised. There may be smaller patches that blend in with the larger rash. The rash may have small bumps and pimples filled with pus. The scrotum in boys may be very red and scaly. The area will itch and cause the child to be fussy.
A combination of factors can result in a candida diaper rash:
-
Not changing dirty diapers. This causes long contact between skin and irritants such as urine and stool. This increases the risk of skin irritation and yeast infection.
-
Diet changes. As a baby grows, food changes can cause changes in the stool. When chemicals in urine mix with this stool, the skin can be affected.
Candida diaper rash is most often treated with over-the-counter antifungal cream or ointment. The rash should clear up a few days after starting the medicine. Infections that don’t go away may need a prescription medicine. In rare cases, a bacterial infection can also occur.
Home care
Medicines
Your child's health care provider will recommend an antifungal cream or ointment for the diaper rash. They may also prescribe a medicine to help relieve itching. Follow all instructions for giving these medicines to your child. Apply a thick layer of cream or ointment on the rash. It can be left on the skin between diaper changes. You can apply more cream or ointment on top, if the area is clean.
General care
Follow these tips when caring for your child:
-
Wash your hands well with soap and clean, running water before and after changing your child’s diaper and applying any medicine.
-
Check your child's diaper often. Change the diaper as soon as you notice it's soiled. Gently pat the area clean with a warm, wet soft cloth. If you use soap, it should be gentle and scent-free. Topical barriers, such as zinc oxide paste or petroleum jelly, can be used. They help by making a barrier between the skin and the diaper, urine, and feces.
-
Don’t over-clean the affected skin areas. This can irritate the skin further.
-
Don’t apply powders, such as talc or cornstarch, to the affected skin areas. Talc can be harmful to a child’s lungs. Cornstarch can cause the candida infection to get worse.
-
Change your child’s diaper at least once at night. Put the diaper on loosely.
-
Use a breathable cover for cloth diapers instead of rubber pants. Slit the elastic legs or cover of a disposable diaper in a few places. This will allow air to reach your child’s skin. Disposable diapers may be preferred until the rash has healed.
-
Let your child go without a diaper for periods of time. Exposing the skin to air will help it heal.
-
Use super-absorbent diapers to minimize exposing the skin to irritants (like urine and feces).
-
If you use baby wipes, make sure the wipes are free of soap, essential oils, fragrances, and harsh detergents that can irritate the skin.
-
Do not use wipes that have alcohol or perfume. They may dry out or irritate the skin more.
-
Avoid using fabric softeners or dryer sheets. They may make the rash worse.
-
Rinse cloth diapers 2 or 3 times to remove all soap or detergent.
Follow-up care
Follow up with your child’s health care provider as directed.
When to get medical advice
Unless your child's health care provider advises otherwise, call the provider right away if your child:
-
Has a fever.
-
Is fussier than normal or keeps crying and can't be soothed.
-
Has symptoms that get worse or don’t get better with treatment.
-
Develops new symptoms, such as blisters, open sores, raw skin, or bleeding.
-
Has abnormal or bad-smelling fluid leaking in the affected skin areas.
Fever and children
There are several different ways to take a child's temperature, including:
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable method but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert the lubricated thermometer gently. You only need to insert the tip of the thermometer (1 cm to 2 cm deep). The readings will still be reliable. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel okay using a rectal thermometer, ask the health care provider what type to use instead. When you talk with any health care provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s provider may give you different numbers for your child. Follow your provider’s specific instructions.
First, ask your child’s provider how you should take the temperature.
Fever readings for a baby under 3 months old:
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the health care provider if this occurs:
-
A repeated temperature of 104°F (40°C) or higher in a child of any age
-
A fever of 100.4° (38°C) or higher in baby younger than 3 months
-
A fever that lasts more than 24 hours in a child under age 2
-
A fever that lasts for 3 days in a child age 2 or older
Featured in