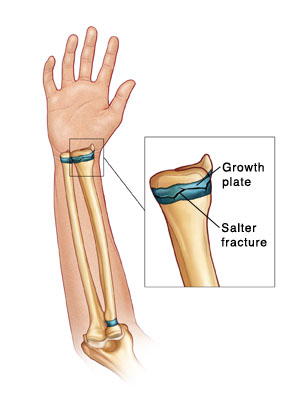
Your child may have a crack or break (fracture) in the growth plate of a bone in their shoulder, arm, or hand. A growth plate is an area near each end of the long bones that exists in children from birth to the teen years. It allows the bone to grow as the child grows. Once the bone’s growth is complete, the growth plate changes to solid bone. A break in the growth plate is known as a physeal, Salter, or Salter-Harris fracture. Health care providers sort growth plate breaks in many ways. The Salter-Harris system is the most common. It grades the break from I to V. The higher the number, the more serious the break.
A normal growth plate can’t be seen on an X-ray. So a break in the growth plate can’t be seen on an X-ray unless the nearby bone is pushed out of place (displaced). Your child may need follow-up X-rays. After this time, if a break is there, new bone growth may be seen on X-ray.
If the second X-ray doesn’t show any sign of a break and your child isn’t in pain, they likely won’t need any treatment. If your child is in pain or the second X-ray shows that a break is there, a splint or cast may be put on the arm or hand. This will hold the bones in place while they heal. The arm may also be put into a sling to raise (elevate) it and hold it still.
Home care
Your child’s provider may prescribe medicines for pain. Follow the provider’s directions for giving these medicines to your child. Don’t give your child aspirin unless the provider tells you to. If pain medicine wasn't prescribed, ask the provider what medicine to give your child for pain or discomfort.
General care
-
Follow the provider’s instructions about how much your child should use the affected arm during the time between X-rays and after an injury is confirmed or ruled out.
-
If the arm is swollen or painful, keep it elevated. As often as possible, lay your baby down and put pillows under the arm until the injured area is raised above the level of the heart. In older children, have the child sit or lie down. Put pillows under the arm until the hand is raised above the level of the heart. For babies and younger children, watch that the pillows don't slip and move near the face.
-
Put a cold pack on the injured area to help control swelling. You can make a cold pack by putting ice cubes in a plastic bag that seals at the top. Wrap the bag in a thin towel. As the ice melts, be careful that the cast or splint doesn’t get wet. Don’t put the ice directly on the skin. This can cause damage. It may be hard to use the cold pack because most children don’t like the feel of the cold. Don’t force your child to accept the ice. This could make both of you miserable. Sometimes it helps to make a game of it.
-
Hold the cold pack on the injured area for up to 20 minutes every 1 to 2 hours the first day. Keep using the cold pack 3 to 4 times a day for the next 2 days, then as needed. You can place the cold pack directly on the splint or cast.
-
If your child is given a splint or cast, care for it as you’ve been advised. Don’t put any powders or lotions inside it. Keep your child from sticking objects into it.
-
Keep the splint or cast completely dry at all times. It should be covered with a plastic bag and kept out of the water when your child bathes. Close the top end of the bag with tape or rubber bands.
-
Encourage your child to wiggle or exercise their fingers on the affected arm often.
Follow-up care
Follow up with your child’s provider as advised. Growth plate fractures often heal well with no problems as long as you maintain regular follow up with your provider as advised. But your child may need to be seen by a specialist. If you were referred to a specialist, make that appointment as soon as you can.
Special note to parents
Health care providers are trained to recognize injuries like this one in young children as a sign of possible abuse. Several providers may ask questions about how your child was injured. Providers must, by law, ask you these questions. This is done for the child's protection. Please try to be patient and not take offense.
Call 911
Call
-
Your child has trouble breathing.
-
Your child appears confused.
-
Your child is very drowsy or has trouble waking up.
-
Your child faints or loses consciousness.
-
Your child has a rapid heart rate.
-
Your child has a seizure.
-
Your child has a stiff neck.
When to contact your doctor
Contact your child's provider right away if:
-
Symptoms like swelling or pain get much worse.
-
Your child has a fever (see "Fever and children" below).
-
Your child has chills.
-
The fingers of the hand on the injured arm are cold, blue, numb, burning, or tingly. If the splint is on, loosen it before going for help. It may be too tight.
-
The swelling or pain gets worse after a cast or splint is put on the arm. Babies too young to talk may show pain with crying that can't be soothed. If the splint is on, loosen it before going for help.
-
The cast or splint gets wet or soft.
-
You have any problems with the splint or cast.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 months old, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The health care provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the provider what type to use instead. When you talk with any provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
Featured in