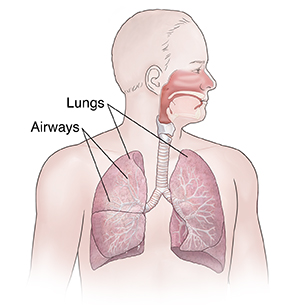
The lungs’ job is to get air into and out of the body. Inside the lungs, air travels through a network of branching airways (tubes) made of stretchy tissue. If something blocks these airways, or if there is too much pressure on a lung, the lung may collapse. Partial or full collapse of a lung is called atelectasis. This can cause a drop in oxygen levels. Atelectasis may be due to any of these:
-
A long time on bed rest.
-
Pattern of shallow breathing.
-
Heavy sedation.
-
Obesity.
-
A foreign object in 1 of the air passages.
-
A tumor (benign or malignant) that presses on an air passage.
-
Chest or belly (abdominal) pain from surgery, injury, or other condition that may limit the ability to cough or breathe deeply.
The treatment for atelectasis depends on the cause.
What are the symptoms of atelectasis?
Atelectasis commonly shows no noticeable symptoms. Underlying conditions, such as COPD, may contribute to the symptoms. When atelectasis affects major lung areas, lowered blood oxygen levels (hypoxemia) may occur. Symptoms may include:
-
Trouble breathing.
-
Shortness of breath.
-
Coughing.
-
Chest pain.
-
Rapid breathing.
-
Skin and lips turning blue.
Home care
If your atelectasis is due to bed rest, sedation, shallow breathing, or obesity, do these things to help increase air flow in your lungs.
-
If you were given an incentive spirometer device: Use it as directed.
-
If you weren't given an incentive spirometer: Take 4 very deep breaths every 1 to 2 hours while awake. As you exhale, purse your lips as if you were blowing up a balloon. (If you have one, you can actually blow up a balloon or a rubber glove.)
If atelectasis was due to other causes, follow your provider’s advice for home care.
Follow-up care
Follow up with your health care provider, or as advised.
When to call your doctor
Contact your health care provider right away if:
-
You have a cough with congestion or colored sputum.
-
You start having belly pain, or it gets worse.
-
You have a fever of 100.4°F (38°C) or higher, or as directed by your provider.
Call 911
Call
-
You are short of breath.
-
You have chest pain that's worse with breathing.
-
You're dizzy, weak, or you faint.
-
You cough up blood.