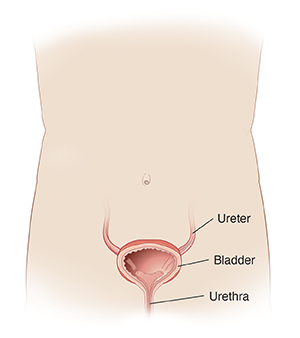
The urethra is the tube that allows urine to pass out of the body. In a woman, the urethra is the opening above the vagina. In men, the urethra is the opening on the tip of the penis. Dysuria is the feeling of pain or burning in the urethra when passing urine.
Dysuria can be caused by anything that irritates or inflames the urethra. An infection or chemical irritation can cause this reaction.
A bladder infection is the most common cause of dysuria in adults. A urine test can diagnose this. A bladder infection needs antibiotic treatment.
Soaps, lotions, colognes, and feminine hygiene products can cause dysuria. So can birth control jellies, creams, and foams. It will go away 1 to 3 days after you stop using these irritants.
Sexually transmitted infections (STIs), such as chlamydia or gonorrhea, can cause dysuria. Your doctor may take a culture sample. Your doctor may start you on antibiotic medicine before the culture test returns.
In women who have gone through menopause, dysuria can be from dryness in the lining of the urethra. This can be treated with hormones. Dysuria becomes long-term (chronic) when it lasts for weeks or months. You may need to see a specialist (urologist) to diagnose and treat chronic dysuria.
Home care
These home care tips may help.
-
Don't use any chemicals or products that you think may be causing your symptoms.
-
If you were given a prescription medicine, take it as directed. Take it until it is all used up.
-
If a culture was taken, don't have sex until you've been told that it is negative. A negative culture means that you don't have an infection. Then follow your doctor's advice to treat your condition.
If a culture was done and it is positive:
-
Both you and your sexual partner may need to be treated. This is true even if your partner has no symptoms.
-
Contact your doctor or go to an urgent care clinic or the public health department to be looked at and treated.
-
Don't have sex until both you and your partner have finished all antibiotics and your doctor says you are no longer contagious.
-
Learn about and use safe sex practices. The safest sex is with a partner who has tested negative and only has sex with you. Condoms can prevent STIs from spreading, but they aren't a guarantee.
Follow-up care
Follow up with your doctor, or as advised. If a culture was taken, you may call as directed for the results. If you have an STI, follow up with your doctor or the public health department for a complete STI screening, including HIV testing. For more information, contact CDC-INFO at 800-232-4636.
When to call your doctor
Contact your doctor right away if:
-
You aren't better after 3 days of treatment.
-
You have a fever of 100.4ºF (38ºC) or higher, or as directed by your doctor.
-
Your back or belly pain gets worse.
-
You can't urinate because of pain.
-
You have new discharge from the urethra, vagina, or penis.
-
You have painful sores on your penis.
-
You have a rash or joint pain.
-
You have painful lumps (lymph nodes) in your groin.
-
You have testicle pain or swelling of the scrotum.